The replacement of maxillary second molars with implants is challenging due to reduced residual bone height and low bone density in the posterior maxillary region near the tuberosity. This complexity increases when replacing these molars as single units. This article presents a series of clinical cases where maxillary second molars were replaced with unitary implants, detailing the challenges and solutions.
- Materials and Methods:
A retrospective study was conducted on patients with short and extra-short implants in the maxillary posterior sectors, with bone density between 200 and 300 Hu (measured using BTI-Scan III software). The study took place in a private clinic in Vitoria, Spain, from January 2017 to December 2018. Data collection and analysis were performed by two researchers. The Shapiro-Wilk test verified the normal distribution of the sample. Implant survival and crestal bone loss were the main variables evaluated. Qualitative variables were described by frequency analysis, and quantitative variables by mean and standard deviation. Implant survival was calculated using the Kaplan-Meier method.
- Results:
Thirty patients received 40 single implants, each 5.5 or 6.5 mm in length, in upper second molar positions that met the inclusion criteria. Most implants were 6.5 mm (60%), followed by 7.5 mm (30%) and 5.5 mm (10%). The mean bone density at the implant sites was 240 Hu (±54; range 200-300 Hu). The mean insertion torque was 40 Ncm (±14.7; range 20-65 Ncm). Mean bone loss was 0.5 mm mesially (±0.6) and 0.3 mm distally (±0.5). The mean follow-up period was 60 months (±34). No implants failed during the follow-up period.
- Conclusions:
Single implants can be successfully used to replace upper second molars, even in cases of bone atrophy and low density. Ensuring success requires following an appropriate surgical and prosthetic sequence. Every step, from initial planning to crown placement, is crucial for achieving optimal treatment outcomes.
- Introduction:
Maxillary posterior edentulism often results in reduced bone height and density due to sinus pneumatization, making implant placement challenging. Short implants have become a minimally invasive, routine option to avoid complex regenerative procedures like sinus lifts, boasting survival rates around 99%. However, the lower bone density in the posterior maxilla complicates the stabilization and integration of short implants, particularly for single crowns.
- Materials and Methods:
A retrospective study was conducted on patients with short and extra-short implants in maxillary posterior sectors, with bone density between 200 and 300 Hu, measured using BTI-Scan III software. The study took place in a private clinic in Vitoria, Spain, from January 2017 to December 2018.
- Surgical and Rehabilitation Protocol:
Residual bone volume was diagnosed using BTI-Scan III software. Patients received amoxicillin and paracetamol before and after surgery. Implants were inserted using a low-revolution biological drilling technique. Panoramic radiographs were taken every 6 months, and periapical radiographs measured crestal bone loss at mesial and distal points using Digora for Windows software.
- Statistical Analysis:
Statistical data collection and analysis were conducted by two researchers. A Shapiro-Wilk test verified the normal distribution of the sample. The primary variable evaluated was implant survival, followed by crestal bone loss. Qualitative variables were analyzed by frequency analysis, and quantitative variables were described using mean and standard deviation. Implant survival was calculated using the Kaplan-Meier method. Data were analyzed using SPSS v15.0 for Windows (SPSS Inc., Chicago, IL, USA).
- Results:
Thirty patients received 40 single implants (5.5 and 6.5 mm) in upper second molar positions. Females constituted 70% of the cohort, with an average age of 62 years (±3.5). Implant distribution was evenly split between teeth 17 and 27. Most implants had a diameter of 5 mm (56.42%), followed by 5.5 mm (23.58%) and 4.5 mm (20%). Lengths were predominantly 6.5 mm (60%), 7.5 mm (30%), and 5.5 mm (10%). Mean bone density at implant sites was 240 Hu (±54; range 200-300 Hu), and mean insertion torque was 40 Ncm (±14.7; range 20-65 Ncm). Average bone loss measured 0.5 mm mesially (±0.6) and 0.3 mm distally (±0.5). Implants were followed up for an average of 60 months (±34) without any failures, achieving 100% survival. No adverse surgical or prosthetic events were recorded.
- Discussion:
Dental implant rehabilitation is highly adaptable to various types of bone atrophy. Short and extra-short implants are effective for vertical atrophy, offering fewer biological complications, lower costs, and fewer surgical sessions than bone augmentation techniques. With a long-term survival rate of 98.9%, these implants perform comparably to longer implants without bone augmentation.
A key challenge is achieving primary stability in the posterior maxilla, essential to prevent micromovements during integration. Using 3D cone-beam imaging helps strategically place implants in areas of highest bone density and tailor the drilling sequence. Studies indicate no significant difference in survival or bone loss between high and low insertion torques.
Effective load transmission and prevention of microleakage are also crucial. Single transepithelial prostheses used in these cases facilitate this, allowing for the fabrication of crowns without excessive heating of the implant connection, ensuring durability and precision.
- Conclusions:
Single implants can effectively replace upper second molars, even in cases of bone atrophy and low density. Success depends on following an appropriate surgical and prosthetic sequence, with careful attention to each step from initial planning to crown placement.



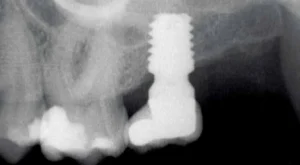
Figure 1 Initial X-ray of the case, where we can see in the second quadrant an edentulous section corresponding to tooth 27 that will be rehabilitated using dental implants.
Figure 2. Placement of the unitary transepithelial after the second phase at 5 months for progressive loading of the implant..
Figures 3-4 Clinical images of the patient at the time of crown placement.
Figure 5. Radiographic image at 4 years of follow-up showing the bone stability of the implant and the rehabilitation
Author : Dr. Eduardo Anitua
Read Article in Dental News